There is no secret that there's a drug overdose crisis in the United States and that opioid overdose deaths have risen 255% from 1999 to 2015. However, in all our flurry to find new technologies or treatments or expand 12 step programs or create drug courts or use Vivitrol to fight this crisis there is one dirty little secret that never gets mentioned in the press: many countries in the world have overcome a huge drug overdose crisis very cheaply using technology which is more than 50 years old. What they have done is to take methadone, an extremely cheap drug which costs less than a dollar a day for a maintenance dose, and make it readily available to everyone everywhere by allowing patients to take their doses in pharmacies and doctor's offices for free. This needs to be the first step we need to take to reverse the overdose crisis in the United States: Change the laws to allow patients to take their dose of methadone in pharmacies and doctor's offices and have the federal government pick up the tab, which is extremely cheap compared to a methadone clinics, drug courts, Suboxone, or 28 day rehabs and which, unlike them, actually works. How do we know it works? Seven countries that overcame an overdose crisis can't be wrong.
In order to find out what works and what doesn't work in fighting an overdose crisis, I looked at data from 33 countries which have published detailed data about drug dependence, overdose, and treatment responses for a long time period. These countries are the United States, Australia, Switzerland, and the 30 countries reporting to the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA). A major overdose crisis was defined as more than 2.0 drug poisoning deaths per 100,000 person years and long term success was greater than 40% reduction in overdose deaths for a minimum of nine years. The seven countries in the world that fit these criteria were Australia, Germany, Greece, Italy, Luxembourg, Norway, and Switzerland. The percentage by which each of these countries reduced their drug related death rate from its peak year until the most recent year for which data is available is given in Figure 1. Figure 2 shows the trends in drug related death rates for each country over the period for which published data is available. US death rates are also given for comparison.
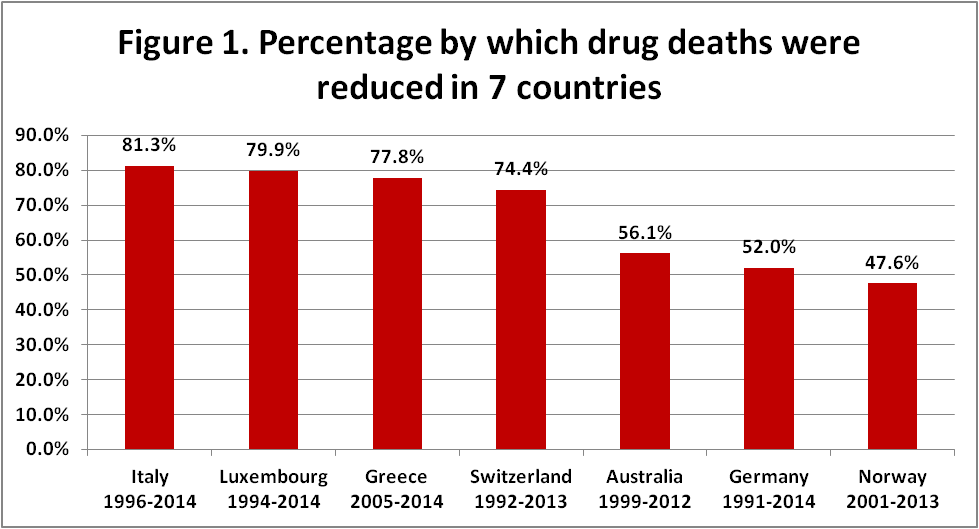
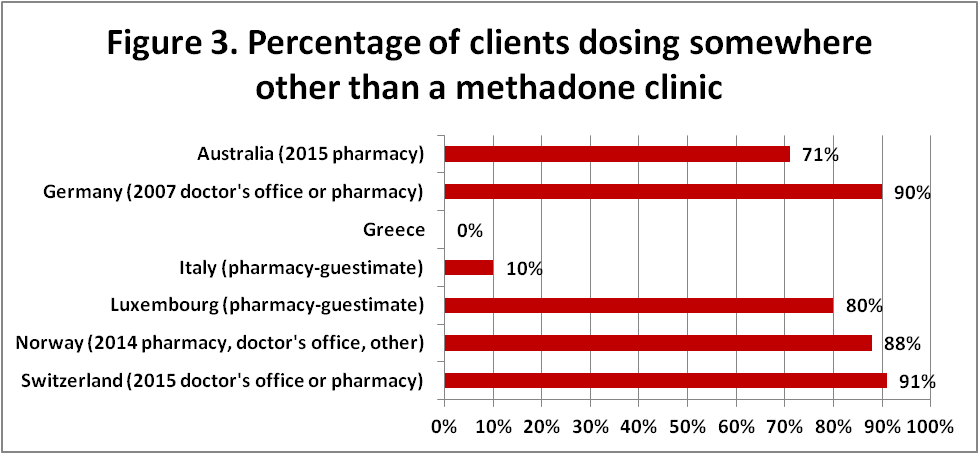
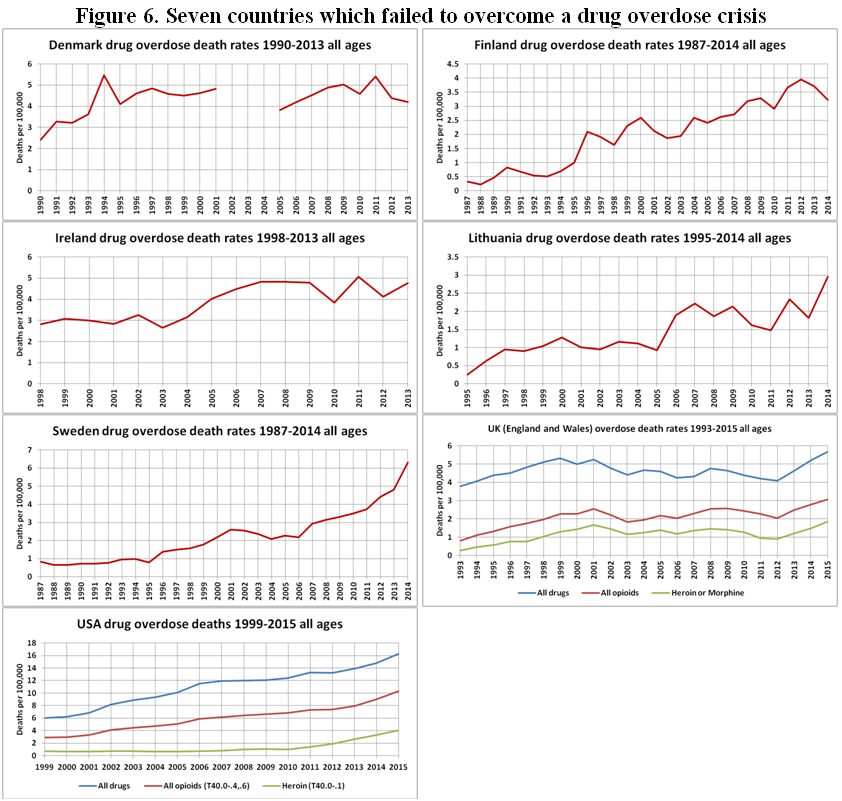
I also identified seven countries which failed to reverse their opioid overdose death rates: Denmark, Finland, Ireland, Lithuania, Sweden, United Kingdom, and United States. In addition to this there are five countries which have had short term success at reversing their overdose crisis; these are Austria, Croatia, Estonia, Malta, and Slovenia. These 12 countries will be discussed later. None of the other countries in the sample had ever had a rate of more than 2.0 overdose deaths per 100,000 person years and so were excluded from this article.
The Seven Biggest Successes
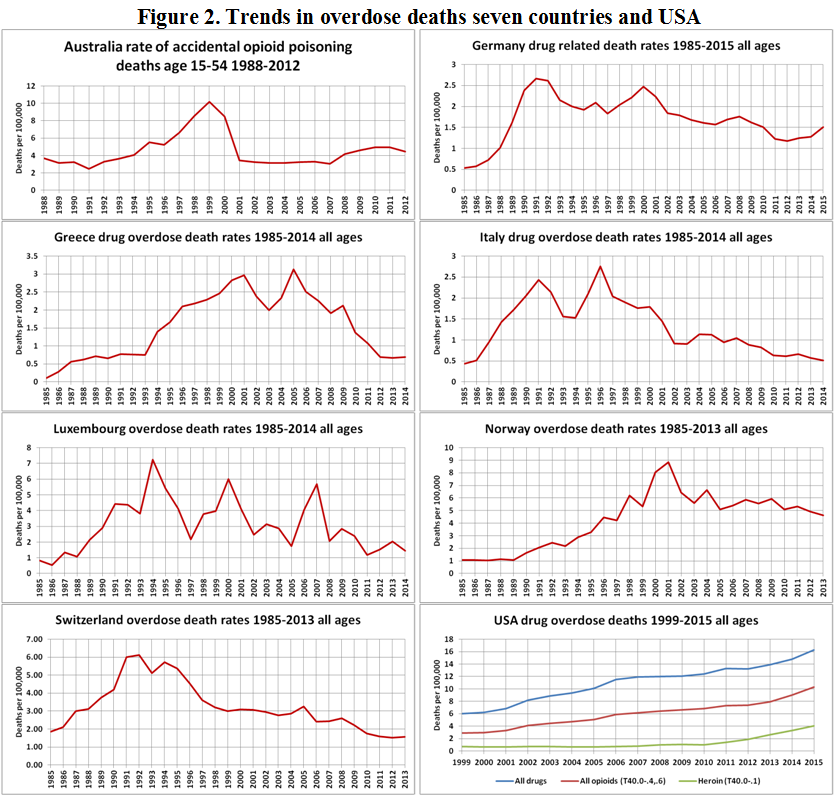
The first task was to identify what these seven successful countries had in common; possible factors were opioid substitution therapy (OST), drug consumption rooms (DCRs), heroin assisted treatment (HAT), housing first initiatives, and take home naloxone (THN). The overwhelming commonality was that all seven countries had extremely good access to opioid substitution therapy (OST) with extremely few barriers. The majority of clients take their dose of methadone or buprenorphine in pharmacies or doctors' offices instead of methadone clinics in five of these countries: Australia, Germany, Luxembourg, Norway, and Switzerland. Although pharmacy based dosing of methadone is legal in Italy it is rare and most methadone and buprenorphine clients have to go to a specialized clinic to dose. Only in Greece are clients required to come to a specialized clinic to dose; clinic dosing is required for both methadone and buprenorphine in Greece. Dosing point statistics are given in Figure 3. For Italy I have estimated that about 10% of clients dose at a doctor's office or pharmacy since the EMCDDA country profile for Italy states that "the provision of OST outside specialized treatment centers (SerDs) is rare."
Moreover, opioid substitution therapy (OST) is essentially free to patients in six out of seven of these countries. Only Australia charges major fees for OST and it is speculated by the Penington Institute (2015) and others that these fees are one reason that overdose deaths have begun to rise again in Australia.
There is generally no wait time for OST in these countries and people are not kicked out of treatment for "dirty" urine samples. Moreover, OST is available for everyone who desires it.
In Australia, Germany, Luxembourg, and Switzerland OST can be initiated in doctor's offices; Greece, Italy, and Norway, however, require that OST be initiated at a specialized treatment center. Once OST is initiated, however, it is usually continued by doctors in office practice in Australia, Germany, Luxembourg, Norway, and Switzerland. Only Greece requires attendance at a specialized treatment clinic (OTP) to continue OST. In Italy most, but not all, clients are required to go to a specialized treatment clinic (OTP) to continue OST.
Some of these countries also have instituted other initiatives to reduce overdose deaths; however, none of these are as widespread and long established as OST.
Drug consumption rooms (DCRs), sometimes called safe injection facilities, undoubtedly save lives but there just aren't enough of them yet. Australia has one DCR (opened 2001), Germany has 24 (the first opened in the early 1990s and they became legally sanctioned in 2000), Luxembourg has one (since 2005), Norway has one (since 2005), and Switzerland has 12 (since 1986). There are none in Greece or Italy. DCRs alone could not have been the factor which turned around the overdose crisis in these countries although they are extremely important life saving programs. Luxembourg and Norway are both slated to open an additional DCR soon.
Heroin assisted treatment (HAT): Out of the seven countries under discussion, only two have HAT: Germany (since 2003) and Switzerland (since 1994). Luxembourg plans to initiate HAT in 2017. Only 0.5% of medication assisted treatment clients are in HAT in Germany and 8% are in HAT in Switzerland.
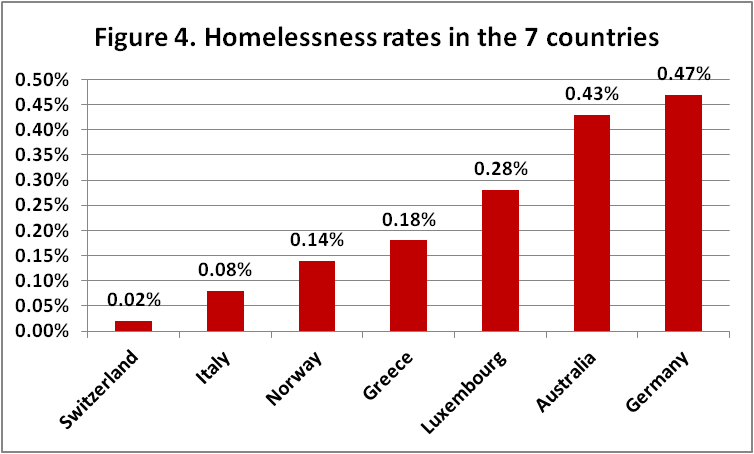
Housing first initiatives undoubtedly decrease drug use and drug overdose deaths; however, rates of homelessness in the seven countries under consideration vary from minimal in Switzerland to appalling in Germany and Australia. Housing cannot account for the reduction in drug deaths in all these seven countries. Homelessness rates are given in Figure 4.
Take home naloxone (THN) programs are found in Australia (since 2011), Germany (since 1999), Italy (since 1996), and Norway (since 2014). There are none in Greece, Luxembourg, or Switzerland. Australia has also made naloxone over-the-counter, although this has also introduced cost issues. THN programs are big lifesavers but because they are not found in all countries under discussion they cannot account for the reductions in overdose in all seven countries.
The evidence suggests that cheap/free and easy access to OST is the most fundamental building block needed to reverse an opioid crisis. Once that foundation is in place, countries will benefit by adding drug consumption rooms, heroin assisted treatment, take home naloxone, and housing first programs to it. But without affordable and accessible OST these other programs alone are insufficient. The way to make OST affordable and accessible in the US is with office based prescribing and pharmacy dosing of methadone which costs less than a dollar a day for the medication itself.
Seven Countries Which Failed To Overcome a Major Opioid Overdose Crisis
We are going to divide these countries into two groups; the first group consists of five countries where the opioid overdose death toll is continuing to spiral out of control and the second group of two countries where the death rates have leveled off due to rational drug and treatment policies.
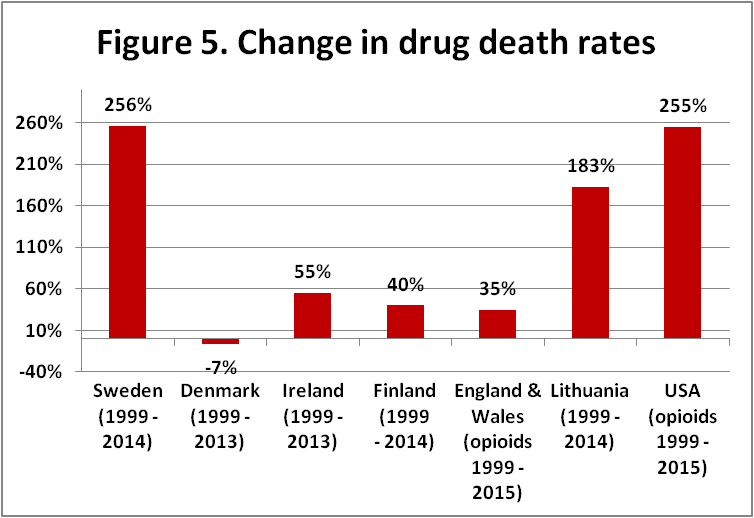
Figure 5 gives the percentage change in drug overdose death rates for each of the seven countries from 1999 to the most recent year for which there is data. Figure 6 shows the trends in death rates over time for the seven countries.
USA
The USA is the worst of any country investigated in this article in terms of overdose deaths. The rate of opioid overdose death in the USA increased 255% between 1999 and 2015. The number of opioid overdose deaths (T40.0-.4,.6) went from 8,050 (2.88 per 100,000) in 1999 to 33,091 (10.3 per 100,000) in 2015. As Jones et al. (2015) have noted in detail, OST coverage is quite inadequate in the US. The payment system is insane with many people not covered by insurance and paying hundreds of dollars out of pocket each month for OST. Moreover in the US people are shamed for being on methadone. We should praise people for going on methadone. Not shame them. The regulations for initiation and dosing of methadone in the US are completely different from those for buprenorphine, unlike most countries in the world which treat these two substitution medications the same. Buprenorphine is far more accessible because it is far more expensive and results in huge profits for big pharma which lobbies for buprenorphine and against methadone. The US has no drug consumption rooms and no HAT. The homelessness rate is fairly low (0.18%) and a lot of housing first initiatives have been put in place. Tiny harm reduction agencies do a truly awesome job of distributing take home naloxone, but it is not enough. Naloxone has been made over-the-counter in 14 states; however, this is not enough. The federal government needs to change the laws to allow office based methadone initiation and pharmacy-based methadone dosing. The federal government needs to subsidize all OST so that it is free for all. This is the first step. After this we need to legalize drug consumption rooms and create a federal initiative to get naloxone into the hands of all drug users and their friends and families at an affordable cost. If big pharma keeps price gouging for naloxone, then pay for the program by fining big pharma. And last but not least we can add HAT once OST is in place.
Sweden
Sweden is the second worst country for overdose deaths as the percentage of increase is essentially the same as that in the US but the current death rate (6.3 per 100,000 for all drugs) is much lower. The rate of overdose death in Sweden increased 256% between 1999 and 2014. As is noted in the EMCDDA country profile for Sweden, Swedish OTPs have "introduced 'zero tolerance' against lateral drug use (i.e. the use of illicit drugs while on OST) which leads to low retention rates in the treatment. In cases of lateral drug use, the clients are frequently referred to another type of treatment." In other words, people are being kicked off methadone and buprenorphine for "dirty" urine tests. Moreover, there has been a decline in the number of clients in OST since 2011. Clients must go to a specialized OTP clinic to dose and to initiate treatment with both methadone and buprenorphine; there is no office-based or pharmacy based dosing or initiation of either.
Sweden has no drug consumption rooms, no take home naloxone, and no HAT. Sweden has high rates of homelessness (0.36%) and inadequate drug user housing. It should come as no surprise that Swedish overdose deaths are out of control.
UK (England and Wales)
Data for England and Wales is taken from the Office for National Statistics since the EMCDDA data are far less complete. Data for Northern Ireland and Scotland is not included. The opioid overdose death rate increased 35% in England and Wales between 1999 and 2015. More shockingly, it increased 51% between 2012 and 2015 and the rate for all drug overdose deaths increased even more over this period. In 2010 the government of the United Kingdom decided to replace the highly effective harm reduction approach to drug use which had been in place for decades with a more politically popular "recovery" approach focused on abstinence and in so doing precipitated a major public health crisis for drug users as has been noted by Middleton et al. (2016) and Ford and Willott (2016). Given the resounding failure of US drug policies, only an idiot, an insane person, or an utterly unscrupulous politician would consider importing them into the UK. The UK has the mechanisms in place for a highly successful drug policy; these include pharmacy dosing and office prescription of OST, take home naloxone, HAT, etc. The only thing missing is drug consumption rooms. As we can see from Figure 6, after a peak in 2001, the UK did a rather good job of reducing or at least containing drug overdose deaths before the policy changes enacted in 2010. What the UK needs to get back on track is to reverse the policy of trying to force people off of methadone and buprenorphine and instead allow them to stay on OST for as long as needed as was done prior to 2010.
Lithuania
Drug overdose death rates increased 183% in Lithuania between 1999 and 2014. The number of deaths went from 37 (1.0 per 100,000) in 1999 to 87 (3.0 per 100,000) in 2014. OST in Lithuania, whether methadone or buprenorphine, can only be dispensed at specialized OTP clinics. OST coverage is poor. A 2007 report estimated there were 5,458 problem opioid users in Lithuania; in 2014 only 585 clients were in OST. This is less than 11% of those in need of OST. 95% of opioid treatment admissions in Lithuania are for heroin. In 2014 in Lithuania 479 OST clients (82%) were receiving methadone and 106 (18%) were receiving buprenorphine.
Lithuania has no drug consumption rooms, no take home naloxone programs, and no heroin assisted treatment (HAT). The homelessness rate for Lithuania was estimated at 0.16% in 2014. Grade B for housing.
Finland
Drug overdose death rates increased 40% in Finland between 1999 and 2014. Number of deaths went from 119 (2.3 per 100,000) in 1999 to 176 (3.2 per 100,000) in 2014. Rates actually peaked in 2012 when there were 213 deaths (3.9 per 100,000) and fell 18% in the following two years; however, there don't seem to have been any major policy or treatment changes which account for this drop.
The primary opioid of abuse in Finland is buprenorphine; according to the 2014 EMCDDA National Report for Finland, buprenorphine accounts for at least 62% of all illicit opioid use and 88% of buprenorphine users inject it. Among clients seeking treatment for problem opioid use in Finland in 2014, 86% were seeking treatment for buprenorphine and only 2% were seeking treatment for heroin. According to the 2014 EMCDDA National Report, buprenorphine was involved in 156 overdose deaths in 2010 whereas heroin was involved in only a handful. About 70% of opioid injectors in Finland inject buprenorphine; the primary source of buprenorphine is from outside the borders of Finland, not diversion.
Although pharmacy dosing of methadone is legal in Finland, only about 7% of people in OST have been given a pharmacy contract and the other 93% must go to a specialized OTP clinic to dose. It is estimated that there were 13,836 problem opioid users in Finland as of 2012, but as of 2014 only 3,000 were in OST, giving a rate of coverage of only 22%. Overall, access to OST in Finland is poor.
Finland has no drug consumption rooms, no take home naloxone programs, and no heroin assisted treatment (HAT). The homelessness rate for Finland was 0.13% as of 2011. Grade B for housing.
Two Countries Where Opioid Overdose Deaths Have Leveled Off
These are Ireland and Denmark.
Ireland
Drug overdose death rates increased 55% in Ireland between 1999 and 2013. The number of deaths went from 115 (3.1 per 100,000) in 1999 to 219 (4.8 per 100,000) in 2013. However, starting in 2007, drug overdose deaths in Ireland stopped increasing and leveled off. There were 209 deaths (4.8 per 100,000) in 2007 and 219 (4.8 per 100,000) deaths in 2013. That the rising tide of deaths was stemmed and leveled off can largely be attributed to improved access to opioid substitution treatment (OST).
The number of OST clients in Ireland increased 165% from 3,689 clients in 1998 to 9,764 clients in 2014. OST is essentially free of charge in Ireland. Methadone can be dispensed in pharmacies and by mobile units as well as in specialized OTP clinics. Interestingly, according to 2014 EMCDDA data, buprenorphine can be dispensed only in specialized OTP clinics. Although buprenorphine was approved for OST in 2002, EMCDDA data from 2014 report that 100% of OST clients in Ireland are on methadone. 89% of opioid treatment admissions in Ireland are for heroin. In 2006 it was estimated there were 20,790 problem opioid users in Ireland, with 9,764 in treatment this gives an estimated treatment coverage of 47%. In 2010 wait times for initiation of methadone treatment varied from 0 to 20.5 months. Average wait time was almost two months.
A take home naloxone pilot project was initiated in Ireland in 2015. Ireland has no drug consumption rooms and no heroin assisted treatment (HAT). The homelessness rate for Ireland was estimated at 0.09% in 2011. Grade A for housing.
Denmark
Drug overdose death rates fell 7% in Denmark from 1999 to 2013. The number of deaths went from 239 (4.5 per 100,000) in 1999 to 235 (4.2 per 100,000) in 2013. 63% of opioid treatment admissions in Denmark in 2011 were for heroin, suggesting the existence of a large prescription opioid abuse problem as well. According to the 2014 EMCDDA National Report for Denmark, in 2013, 23% of all drug poisoning deaths were caused by heroin/morphine or heroin/morphine in combination with another substance, whereas 59% of the poisonings were caused by methadone or methadone in combination with another drug. 18% of the poisonings were caused by other drugs. This is a reversal of the situation in the 1990s when heroin was found in most overdose deaths in Denmark. This suggests the existence of a large methadone abuse problem in Denmark.
OST in Denmark can be dispensed at specialized OTP clinics, pharmacies, or mobile units. Office based initiation of OST is the standard. In 2011, there were 6,200 clients (82%) on methadone and 1,400 clients (18%) on buprenorphine.
Denmark has 5 drug consumption rooms. Take home naloxone has been available since 2013. Heroin Assisted treatment (HAT) has been available since 2009.There were 198 clients in HAT in 2013. As of 2015, the homelessness rate in Denmark was 0.11%. Grade B for housing.
Although Denmark appears to be doing everything correctly, the death rate has essentially leveled off rather than fallen.
Five Countries with Short Term Success in Reducing Overdose Death Rates
Figure 7 shows the five countries which have lowered drug related deaths in the short term, i.e. less than 9 years, compared to the USA.
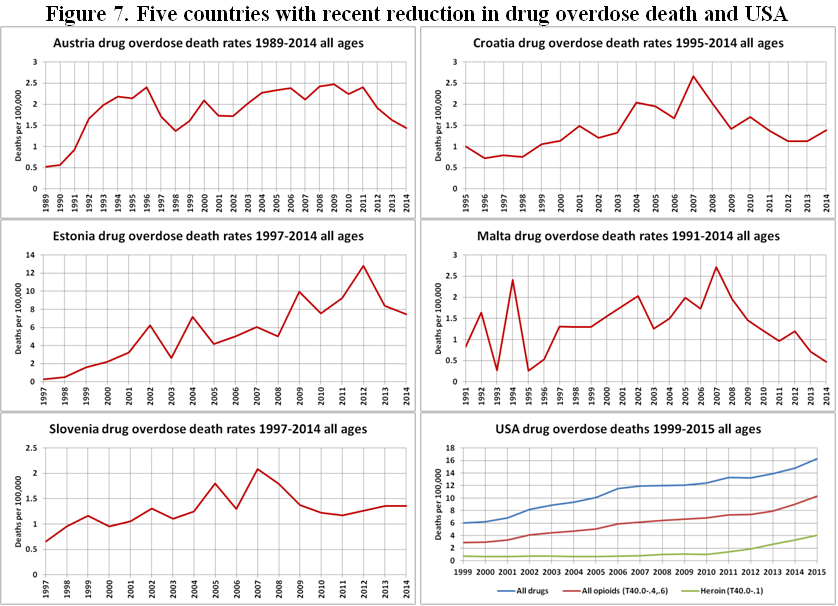
Estonia
Drug overdose death rates dropped 42% in Estonia in the two year period from the peak in 2012 until 2014. Estonia, on their EMCDDA country profile page, attributes this in large part to the take home naloxone program introduced in 2013. According to the 2014 Estonian National Report, "In total, 554 participants received training and 552 naloxone syringe sets were given out during the period of September 2013 - June 2014. 72 repeated prescriptions were reported (one of them was reported as not intended for medical use). Most of the syringes were distributed to users of narcotic substances."
Drug overdose deaths went from 170 (12.8 per 100,000) in 2012 to 98 in 2014 (7.4 per 100,000). Of the 98 deaths in 2014, 92 were attributed to overdose by synthetic opioids, fentanyl and 3-methylfentanyl in particular. According to the 2016 EMCDDA Statistical Bulletin, 86% of opioid treatment admissions in Estonia in 2014 were for fentanyl.
OST is only available at specialized OTP clinics in Estonia. All OST in Estonia is methadone and funded by the state. Estonia has no drug consumption rooms and no heroin assisted treatment (HAT). A 2006 study estimated the number of homeless people in Estonia as 3,500 yielding a homelessness rate of 0.26%. Grade C for housing.
Austria
Drug overdose deaths dropped 42% in Austria in the 5 year period from 2009 to 2014. In 2009 the legal framework around OST, in Austria was revised to allow for much greater ease of access. The number of clients in OST in Austria increased 22%, from 14,202 in 2009 to 17,272 in 2014. At the same time the number of drug overdose deaths dropped from 206 (2.5 per 100,000) in 2009 to 122 (1.4 per 100,000) in 2014. In 2014, of the 17,272 clients receiving OST, 9,591 (56%) received slow-release morphine, 3,599 (21%) received methadone, 3,784 (22%) received buprenorphine-based medications, and the remainder another drug. Office based prescribing of OST is the norm in Austria as is pharmacy based for OST. In 2014, 83% of opioid treatment admissions in Austria were for heroin according to the 2016 EMCDDA Statistical Bulletin.
Austria has no drug consumption rooms, no take home naloxone programs, and no heroin assisted treatment (HAT). There are no estimates of current homelessness rates. The success in overdose reduction in Austria can be largely attributed to improved access to OST.
Malta
Drug overdose death rates dropped 83% in Malta in the 7 year period from 2007 to 2014. Overdose deaths dropped from a peak of 11 deaths (2.7 per 100,000) in 2007 to 2 deaths (0.5 per 100,000) in 2014. One must be very careful in drawing conclusions from such a small population as fluctuations due to random chance can have a major effect. However, it is worth noting that Malta changed its OST laws in 2005 to allow for take home doses of methadone and in 2006 to allow buprenorphine treatment. However, in spite of this, the number of clients in OST in Malta decreased 7% from 1,087 in 2007 to 1,013 in 2014. One may hypothesize that the availability of take home doses increased OST compliance, reduced lateral drug use, and hence reduced overdose deaths. It would be good to conduct a study to investigate if this were true. There is only one specialized OTP clinic in Malta; this clinic dispenses both methadone and buprenorphine. Office based buprenorphine treatment is also available. Methadone is only available through clinic dispensing.
Malta has no drug consumption rooms, no take home naloxone programs, and no heroin assisted treatment (HAT). There are no estimates of current homelessness rates for Malta.
Croatia
Drug overdose death rates dropped 48% in Croatia in the 7 year period from 2007 to 2014. Overdose deaths dropped from a peak of 115 deaths (2.7 per 100,000) in 2007 to 59 deaths (1.4 per 100,000) in 2014. OST clients in Croatia increased 241% from 2,016 in 2007 to 6,867 in 2014. Both office based dosing and clinic based dosing of methadone are available in Croatia. For buprenorphine, clinic based dosing, office based dosing, and pharmacy based dosing is available. Buprenorphine was introduced in 2006. According to the 2014 EMCDDA National Report for Croatia, "Since 2006 the costs of buprenorphine pharmacotherapy of addicts has been borne by the Croatian Health Insurance Fund." Suboxone (buprenorphine + naloxone) was introduced in 2009. Of clients receiving pharmacotherapy for opioid use disorder in 2013, 41% received methadone, 42% received buprenorphine or Suboxone, and the rest received something else. 95% of admissions for opioid treatment were for heroin.
Croatia has no drug consumption rooms, no take home naloxone programs, and no heroin assisted treatment (HAT). The rate of homelessness in Croatia was 0.23% in 2015. Grade C for housing. Reduction in overdose deaths in Croatia is most likely due to improved access to OST.
Slovenia
Drug overdose death rates dropped 35% in Slovenia in the 7 year period from 2007 to 2014. Overdose deaths dropped from a peak of 42 deaths (2.1 per 100,000) in 2007 to 28 deaths (1.4 per 100,000) in 2014. OST clients increased only 8% from 2,957 clients in 2007 to 3,190 in 2014; in fact, the number of OST clients peaked at 3,526 in 2010 and has been falling ever since. As we discuss below, the falling death rates are most likely due to a loss of interest in opioids in Slovenia rather than to treatment or harm reduction responses. In Slovenia, OST dosing can be done at OTPs, doctor's offices, or pharmacies. Interestingly, although methadone dosing can be done at pharmacies, buprenorphine dosing cannot. OST can be initiated at OTPs or doctor's offices. In 2013, of 3,261 OST clients, 2,042 (63%) received methadone, 431 (13%) received Suboxone (buprenorphine + Naloxone), 461 (14%) received buprenorphine (Subutex) and 327 (10%) received slow release morphine.
Slovenia estimates that there has been a general reduction in high risk opioid users and people who inject drugs in recent years. There are fewer young people using or injecting opioids and the population of high risk opioid users is an aging population. It is estimated that there were 10,654 high risk drug users in Slovenia in 2004; this number has dropped to 6,100 in 2011. Thus, the drop in opioid overdose deaths is most likely due to a drop in the number of users rather than to any treatment or harm reduction response. Since there are more new clients seeking treatment for cannabis and fewer new clients seeking treatment for opioids, this suggests that cannabis may be replacing opioids in popularity and leading to fewer overdose deaths.
Slovenia has no drug consumption rooms, no take home naloxone programs, and no heroin assisted treatment (HAT). The homelessness rate in Slovenia was 0.02% in 2014. Grade A for housing. The 2014 National Report for Slovenia states that, "Precarious living arrangements or homelessness were present in 6.3% of drug users who entered the program for the first time, and in 12.3% of users re-entering the program."
Conclusion
As the National Institute for Health points out, the gold standard for determining the effectiveness of an intervention is whether or not it works when implemented in a real life situation, not how it performs in a laboratory. Cheap and easy access to OST has repeatedly in country after country proven effective at stemming or reversing an opioid overdose crisis. And the cheapest way to reach the most people in country as spread out as the US is with pharmacy based dosing of methadone which costs less than a dollar a day. The worst possible approaches are the 28 day rehab or incarceration, since it is a proven fact that both 28 day rehab and incarceration raise the odds of overdose death exponentially. Graduates of 28 day rehabs are 30 times more likely to die of overdose than active heroin users. However, it is essential that the bedrock of cheap and easy access to methadone is in place so that drug consumption rooms, heroin assisted treatment, take home naloxone programs, and housing first initiatives can have a firm foundation to rest upon.
In fact, in 2007 a pilot study of office based prescribing and pharmacy based dosing of methadone was conducted in the US. Clients loved it, doctors loved it, and pharmacists loved it. The only people who hated it were the greedy bastards who owned the methadone clinics and the 28 day rehabs. Well the time has come for us to stand up to the greedy bastards who are killing our children and demand office based prescribing and pharmacy based dosing of methadone today!