Introduction
Although heavy drinking can cause a great deal of health damage ranging from cirrhosis of the liver to pancreatitis, horror stories of alcoholic brain damage are largely a myth. Although wet brain is real, it can be prevented by proper nutrition and is not directly caused by alcohol itself.
Alcohol, Brain Cells, and Brain Shrinkage
It has long been an established fact that actively drinking, alcohol dependent subjects have smaller brain volumes than normal control subjects who do not drink alcohol. Early researchers assumed that this was because alcohol killed the brain cells of alcohol dependent subjects, but current research proves that this hypothesis is largely untrue. Unless there has been brain damage as a result of liver failure or thiamine deficiency, the majority of brain cells of heavy drinkers are intact even though the brain has shrunk. We have also discovered that a long period of abstinence or moderate drinking tends to restore the volume of heavy drinker's brains back to normal.
The human brain consists of white cells and gray cells. The gray cells are responsible for thinking and feeling and decisions--they correspond to the Central Processing Unit (CPU) of your computer. The white cells are like the cables of your computer which connect the keyboard and the monitor to the CPU. In 1993 Jensen and Pakkenberg did brain cell counts which compared the number of cells in the brains of heavy drinkers with those of nondrinkers. What they found was that the number of gray cells was the same in both the heavy drinkers and the nondrinkers. However, there were fewer white brain cells in the brains of the drinkers which implies that alcohol kills white brain cells.
In 2009 George Fein discovered that there was one part of the brain in the parietal lobe--which is associated with spatial processing--where alcohol kills gray cells. Fein claims that this explains why even after alcohol dependent subjects regain use of all their other cognitive functions they still seem to have difficulties with spatial processing.
Studies by Pfefferbaum (1995, 1998) show that with long periods of abstinence or moderate drinking the brains of alcoholic dependent subjects return to nearly the same size as their nondrinking counterparts.
It is not conclusive whether shrinkage is more pronounced in males, in females, or the same in both (Hommer, 2003).
To summarize: The brains of long term, heavy drinkers shrink, but they return to almost full normal size after a long period of abstinence or moderate drinking. Long-term, heavy drinking kills some white brain cells and some of the gray cells responsible for spatial processing; however, it does not kill any other gray cells. In particular, the gray cells which are responsible for our thinking, decision making, and other cognitive processes remain intact even in long-term, heavy drinkers. Unless there is brain damage which is due to thiamine deficiency or liver failure nearly all brain functions of alcohol dependent drinkers can be returned to normal with a long period of abstinence or moderate drinking. Cognitive functioning tends to return to normal when brain size returns to normal.
There is some evidence that both the amount of brain shrinkage and the amount of cognitive deficit are dependent on the quantity of alcohol consumed and the number of years of heavy drinking; it is not established whether this relationship is linear or not.
Amnesia and Dementia Due To Thiamine Deficiency - Wernicke-Korsakoff Syndrome Aka Wet Brain
The condition known as wet brain or Wernicke-Korsakoff Syndrome is a form of brain damage which is characterized by severe amnesia, confabulation, and sometimes dementia (Emsley, et al. 1996). It is not caused by direct effects of alcohol on the brain. It is caused by a severe deficiency of Thiamine (vitamin B1) and is often precipitated by a sudden influx of glucose. A number of things have been shown to lead to a severe enough thiamine deficiency to trigger wetbrain. These include a diet consisting solely of polished rice, prolonged bouts of morning sickness, bulimia and severe alcohol dependence.
Wetbrain has a sudden onset--it is not something which happens gradually over time. The first stage of wetbrain is called Wernicke's encephalopathy. When there is a sudden influx of glucose in a brain which is deprived of thiamine the brain cells begin to die. This is because the chemical reactions which supply these brain cells with energy for life use thiamine to turn glucose into energy in a chemical process called the Krebs cycle. When there is an influx of glucose and no thiamine to help metabolize it, these brain cells burn out like a car engine running on high octane gasoline at high speed with no oil. The brain cells which die first are the ones which require the most thiamine to function. These brain cells are located around the middle of the brain and are the brain cells which are associated with memory and muscular movement. The brain cells of the cerebellum, which controls balance, are also affected.
The symptoms of Wernicke's encephalopathy are confusion, lack of coordination, and involuntary eye movements. If Wernicke's encephalopathy is immediately treated with thiamine it can be stopped and largely reversed. However, if Wernicke's encephalopathy is not immediately treated, it quickly turns into Korsakoff's psychosis, which is permanent and largely resistant to treatment. Symptoms of Korsakoff's syndrome include loss of past memories, inability to learn new things, confabulation (remembering things which never happened), lack of coordination and unsteady gait, and in severe cases dementia. In some cases physicians who should have known better have precipitated Wernicke-Korsakoff syndrome in patients by putting them on a glucose drip instead of a thiamine drip.
Alcohol tends to block absorption of thiamine by the human body, so all people who drink alcohol should be careful to eat well and should also take vitamin B1 pills to make sure that they are getting enough thiamine. Severely heavy drinkers who consume around a fifth or a quart of vodka per day are often too nauseous too nauseous to eat well and may tend to vomit up what they do eat. Moreover, if these people are living on the streets, they may be unwilling to spend money on food which could be used to buy alcohol. These people are in the greatest danger of developing Wernicke-Korsakoff syndrome.
Breedlove (2007) tells us that all cases of wetbrain due to alcohol ingestion could be prevented by regulations requiring that thiamine be added to alcoholic beverages. It is unfortunate that our puritanical US society prefers to send people to abstinence-based programs which fail rather than to eliminate much human suffering by implementing the simple harm reduction policy of adding thiamine to alcoholic beverages.
HAMS recommends that all drinkers be sure to eat nutritious meals and take vitamins--especially thiamine--to help ward off wetbrain. It is also good to try and have some abstinence days or otherwise reduce alcohol intake to help prevent this.
Wetbrain is sometimes complicated by hepatic encephalopathy.
Hepatic Encephalopathy
Hepatic encephalopathy is damage to the brain which is a result of liver failure, which may be caused by cirrhosis, hepatitis, etc. One job of the liver is to screen out toxins so that they can be disposed of as waste rather than circulate in the blood and damage delicate tissues like the brain. When the liver fails it is believed that toxins like ammonia and manganese cross the blood-brain barrier and cause damage to the brain--i. e. hepatic encephalopathy.
Symptoms of hepatic encephalopathy include lethargy, apathy, disorientation, inappropriate behavior, and slurred speech. In severe cases there may be coma.
If alcohol causes liver failure then hepatic encephalopathy can be one result.
Alcohol and Cognitive Dysfunction
People who drink massive quantities of alcohol suffer brain shrinkage and cognitive dysfunction as a result. However, the good news is that if these heavy drinkers do not have thiamine-related brain damage or liver-related brain damage then this cognitive dysfunction and brain shrinkage is almost entirely reversible with a change from heavy drinking to reduced drinking or alcohol abstinence.
Although most researchers emphasize alcohol abstinence, research from Sullivan et al (2000b) demonstrates that reduced drinking also restores cognitive function in formerly alcohol dependent drinkers: abstinence is not the only solution
The data in Table 1 is a conflation of information contained in two papers by George Fein about recovery of cognitive function after stopping heavy drinking. One paper is a literature review published in 1990 and the other is a study published in 2006.
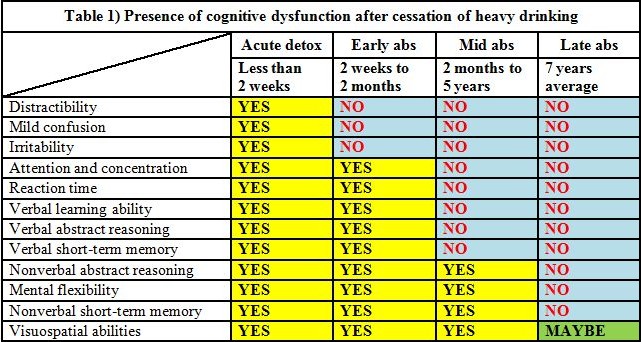
Although Fein's 1990 paper gives a spread of two months to five years for mid stage recovery of cognitive function, Fein's 2006 paper narrows this down and tells us that that these cognitive functions are generally recovered at the end of the first year after ceasing heavy drinking. Parsons (1998) states that remission of cognitive dysfunction occurs at 4 to 5 years.
In Fein's 2006 study the male drinkers at their peak drinking consumed 361.8 ± 257.2 standard drinks per month for a period of 51.0 ± 30.9 months. The female drinkers at their peak consumed 264.0 ± 202.8 standard drinks per month for a period of 92.1 ± 81.2 months. (One standard drink = 14g ETOH.) This is around a half a liter of vodka (80 proof) per day every day for the men and around a "pint" (375 ml) of vodka per day every day for the women. Control subjects averaged less than half a drink per day.
According to Parsons 1998 there is no significant deference between alcohol dependent males and females on the variable of cognitive dysfunction.
Although the dose, the frequency, and the duration of alcohol consumption all appear to have an effect on the degree of cognitive dysfunction (as well as degree of incoordination) the relationship is not entirely clear cut. Parsons (1998) proposes a nonlinear, tripartite, threshold model of the effect of alcohol dose on cognitive dysfunction as exemplified in Table 2.
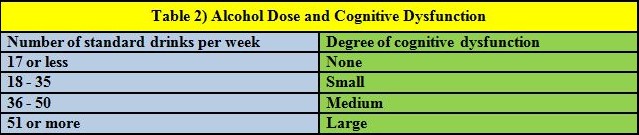
(Note: In their original paper Parson and Nixon used the old definition of a US standard drink--12g ETOH. This has been corrected to the current 14g definition here.)
Sullivan (2000c) tells us that light relapsers performed comparably to abstinent subjects on cognitive tests at the mid stage period of recovery of cognitive function which suggests that reduced drinking may be as good a strategy as abstinence for the recovery of cognitive function in formerly dependent drinkers.
We should also note that these cognitive deficits are present statistically--when we look at actual individuals there are some alcohol dependent subjects in acute detox stage who show better cognitive function than some normal controls--it is just that they are a small minority. Parsons (1998) found 85% discrimination between the control group and the alcohol dependent group when the means of several tests were taken into account. This means that 15% of the alcohol dependent subjects were showing cognitive functioning equal to that of the controls.
In summary: Heavy drinkers who consume around a quart of booze or so every day suffer from cognitive defects and brain shrinkage. When these heavy drinkers quit drinking or reduce their consumption of alcohol to reasonable levels most of these cognitive dysfunction and much of this brain shrinkage goes away by the end of the first year. Virtually all of the cognitive dysfunction and brain shrinkage is gone at the at the end of five or so years except for some loss of white matter, a small loss of gray matter which controls spatial processing, and some minor dysfunction of spatial processing in some individuals. This is true for heavy drinkers who do not have thiamine related brain damage or brain damage related to liver failure which are permanent.
Conclusion
We should have learned long ago that scare tactics based on lies not only fail, but backfire and lead to worse problems than before. When kids found that "Reefer Madness" was a lie they stopped believing warnings about heroin, too. Since we know that drunkards like Hemingway, O'Neill, Faulkner and Steinbeck managed to win the Nobel Prize in Literature in spite of their drinking habits this puts a lie to the myth that every drinker turns into a brain damaged idiot. The time to put an end to the lies is now. Drinking a fifth of liquor a day is clearly not good for your health, but if you watch your nutrition and keep a handle on things then occasionally engaging in recreational intoxication is not nearly so bad as the fear-mongers would lead us to believe.
Lying to kids by telling them that a single night of heavy drinking will turn their brain into a walnut is irresponsible. Kids observe adults engaging in occasional recreational intoxications without suffering major brain damage and they know that they are being lied to. Once you lie to kids you lose your credibility for good because kids are real black and white thinkers. Once you have cried wolf then kids will not believe you when you warn them about real dangers like drinking and driving, the addictive nature of heroin, or the fact that drinking a fifth of liquor a day can rot your liver.
Let's stop all the scare tactics and tell kids the truth for a change--okay?
The life you save may be your child's.
REFERENCES:
Breedlove SM, Rosenzweig MR, Watson NV. (2007). Biological Psychology: An Introduction to Behavioral, Cognitive, and Clinical Neuroscience. Fifth Edition. Sinauer Associates, Inc.
Dlugos, CA and Pentney, RJ. (1997). Morphometric evidence that the total number of synapses on Purkinje neurons of old F344 rats is reduced after long-term ethanol treatment and restored to control levels after recovery. Alcohol and alcoholism (Oxford, Oxfordshire) 32 (2), 161-72
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/9105510
PMID:9105510
Free Full Text: http://alcalc.oxfordjournals.org/content/alcalc/32/2/161.full.pdf
Emsley, R. et al. (1996). Magnetic resonance imaging in alcoholic Korsakoff's syndrome: evidence for an association with alcoholic dementia. Alcohol and alcoholism (Oxford, Oxfordshire) 31 (5), 479-86
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/8949964
PMID:8949964
Free Full Text: http://alcalc.oxfordjournals.org/content/alcalc/31/5/479.full.pdf
Fama, R Marsh, L and Sullivan, EV. (2004). Dissociation of remote and anterograde memory impairment and neural correlates in alcoholic Korsakoff syndrome. Journal of the International Neuropsychological Society: JINS. 10 (3), 427-41
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/15147600
PMID:15147600
doi:10.1017/S135561770410310X
Fama, R et al. (2007). Upper and lower limb motor impairments in alcoholism, HIV infection, and their comorbidity. Alcoholism, clinical and experimental research. 31 (6), 1038-44
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/17403062
PMID:17403062
doi:10.1111/j.1530-0277.2007.00385.x
Fama, R Pfefferbaum, A and Sullivan, EV. (2004). Perceptual learning in detoxified alcoholic men: contributions from explicit memory, executive function, and age. Alcoholism, clinical and experimental research. 28 (11), 1657-65
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/15547452
PMID:15547452
Fein, G et al. (2009). Parietal gray matter volume loss is related to spatial processing deficits in long-term abstinent alcoholic men. Alcoholism, clinical and experimental research. 33 (10), 1806-14
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/19645730
PMID:19645730
doi:10.1111/j.1530-0277.2009.01019.x
Fein, G et al. (2006). Cognitive performance in long-term abstinent alcoholic individuals. Alcoholism, clinical and experimental research. 30 (9), 1538-44
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/16930216
PMID:16930216
doi:10.1111/j.1530-0277.2006.00185.x
Free Full Text: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1868685/pdf/nihms20940.pdf
Fein, G et al. (1990). Cognitive impairments in abstinent alcoholics. The Western journal of medicine. 152 (5), 531-7
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/2190421
PMID:219042
Free Full Text: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1002406/pdf/westjmed00117-0069.pdf
Harper, C and Kril, J. (1991). If you drink your brain will shrink. Neuropathological considerations. Alcohol and alcoholism. (Oxford, Oxfordshire). Supplement 1, 375-80
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/1845566
PMID:1845566
Harper, C and Kril, J. (1994). An introduction to alcohol-induced brain damage and its causes. Alcohol and alcoholism. (Oxford, Oxfordshire). Supplement 2, 237-43
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/8974342
PMID:8974342
Hommer, DW. (2003). Male and female sensitivity to alcohol-induced brain damage. Alcohol research & health : the journal of the National Institute on Alcohol Abuse and Alcoholism. 27 (2), 181-5
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/15303629
PMID:15303629
Free Full Text: http://pubs.niaaa.nih.gov/publications/arh27-2/181-185.pdf
Jensen, GB and Pakkenberg, B. (1993). Do alcoholics drink their neurons away? Lancet. 342 (8881), 1201-4
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/7901529
PMID:7901529
Moselhy, HF Georgiou, G and Kahn A. (2001). Frontal lobe changes in alcoholism: a review of the literature. Alcohol and alcoholism. (Oxford, Oxfordshire) 36 (5), 357-68
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/11524299
PMID:11524299
Free Full Text: http://alcalc.oxfordjournals.org/content/alcalc/36/5/357.full.pdf
Oscar-Berman, M and Marinković, K. (2007). Alcohol: effects on neurobehavioral functions and the brain. Neuropsychology review. 17 (3), 239-57
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/17874302
PMID:17874302
doi:10.1007/s11065-007-9038-6
Oscar-Berman, M et al. (Apr 2004). Comparisons of Korsakoff and non-Korsakoff alcoholics on neuropsychological tests of prefrontal brain functioning. Alcoholism, clinical and experimental research. 28 (4), 667-75
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/15100620
PMID:15100620
Parsons, OA. (1998). Neurocognitive deficits in alcoholics and social drinkers: a continuum? Alcoholism, clinical and experimental research. 22 (4), 954-61
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/9660328
PMID:9660328
Parsons, OA and Nixon, SJ. (1998). Cognitive functioning in sober social drinkers: a review of the research since 1986. Journal of studies on alcohol. 59 (2), 180-90
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/9500305
PMID:9500305
Pfefferbaum, A et al. (Oct 1995). Longitudinal changes in magnetic resonance imaging brain volumes in abstinent and relapsed alcoholics. Alcoholism, clinical and experimental research. 19 (5), 1177-91
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/8561288
PMID:8561288
Pfefferbaum, A et al. (1998). A controlled study of cortical gray matter and ventricular changes in alcoholic men over a 5-year interval. Archives of general psychiatry. 55 (10), 905-12
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/9783561
PMID:9783561
Salen, PN. Wernicke Encephalopathy. eMedicine.
http://emedicine.medscape.com/article/794583-overview
Accessed October 29, 2009.
Sullivan, EV and Marsh, L. (2003). Hippocampal volume deficits in alcoholic Korsakoff's syndrome. Neurology. 61 (12), 1716-9
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/14694035
PMID:14694035
Sullivan, EV et al. (2000). Cerebellar volume decline in normal aging, alcoholism, and Korsakoff's syndrome: relation to ataxia. Neuropsychology. 14 (3), 341-52
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/10928737
PMID:10928737
Sullivan, EV Rosenbloom, MJ and Pfefferbaum. A. (2000). Pattern of motor and cognitive deficits in detoxified alcoholic men. Alcoholism, clinical and experimental research. 24 (5), 611-21
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/10832902
PMID:10832902
Sullivan, EV et al. (2000). Longitudinal changes in cognition, gait, and balance in abstinent and relapsed alcoholic men: relationships to changes in brain structure. Neuropsychology. 14 (2), 178-88
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/10791858
PMID:10791858
Sullivan, EV et al. (2002). Speed and efficiency but not accuracy or timing deficits of limb movements in alcoholic men and women. Alcoholism, clinical and experimental research. 26 (5), 705-13
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/12045480
PMID:12045480
Sullivan, EV et al. (2002). A profile of neuropsychological deficits in alcoholic women. Neuropsychology. 16 (1), 74-83
PubMed Abstract: http://www.ncbi.nlm.nih.gov/pubmed/11853359
PMID:11853359
Wolf, DC. Encephalopathy, Hepatic. eMedicine.
http://emedicine.medscape.com/article/186101-overview
Accessed October 29, 2009.
Xiong, GL. Wernicke-Korsakoff Syndrome. eMedicine.
http://emedicine.medscape.com/article/288379-overview
Accessed October 29, 2009.